8 Types of Abnormal Menstruation — What Your Period Is Trying to Tell You
Your menstrual cycle is one of the body’s most important vital signs. And just like with your heart rate or blood pressure, irregularities should not be ignored. When something about your period feels “off,” it might be your body’s way of signaling an underlying problem — a hormone imbalance, nutritional deficiency, or potential illness.
That’s why I encourage woman to go beyond symptom suppression and begin exploring why they are experiencing irregular cycles in the first place.
In this guide, we’ll look at the eight common types of abnormal menstruation, what they might be telling you about your health, and how you can use nutrition and lifestyle habits to support a more regular, balanced cycle.
What’s Considered a Normal Menstrual Cycle?
A “normal” cycle will vary from woman to woman — what’s important is knowing what is normal for you. In most circumstances, a typical cycle:
Lasts between 24 and 35 days
Includes 3–7 days of bleeding
Should arrive at fairly regular intervals
Comes with minimal pain or disruption
I recommend the practice of “cycle tracking” not only for predicting fertility or as a natural contraceptive but — even more importantly — as a method for understanding your baseline cycle. This way, when it changes or begins to feel different than usual, you’ll be ready to ask for support.
What Causes Menstrual Irregularities?
Irregular periods can be confusing and frustrating — particularly when the catch-all solution so often is “go on birth control.” While hormonal fluctuations are certainly involved (and while hormonal birth control can ease the swings), they rarely occur in a vacuum.
Your menstrual health is influenced by your nutrient intake, your metabolism, your mental health, and more. From a holistic perspective, it’s important to look deeper than the symptoms to understand what’s causing the imbalance.
Conventional Causes of Irregular Periods:
Medical diagnoses often associated with abnormal menstruation include:
PCOS (Polycystic Ovary Syndrome) — marked by irregular or absent ovulation
Thyroid dysfunction — both hypothyroidism and hyperthyroidism can disrupt your cycle
Endometriosis or fibroids — can contribute to pain, heavy bleeding, or spotting
Perimenopause — natural hormonal changes that begin in your 30s or 40s
While these diagnoses are real and important, they don’t always explain why your hormones became dysregulated in the first place — which is where a holistic approach can add value.
Holistic & Functional Causes
From a functional nutrition lens, menstrual irregularities often stem from:
Blood sugar instability — Frequent energy crashes, sugar cravings, and mood swings may signal imbalances that interfere with ovulation and hormone production.
Under-eating or over-exercising — Too few calories, carbs, or fats — or too much physical stress — can suppress your body’s reproductive function.
Chronic stress — Elevated cortisol levels from emotional, physical, or environmental stressors can throw off your hormonal rhythm and delay or disrupt ovulation.
Nutrient deficiencies — Inadequate intake of key vitamins and minerals (like magnesium, B6, zinc, and iron) can hinder hormone production and detoxification.
Poor liver or gut function — A sluggish liver or imbalanced gut can impair your body’s ability to eliminate excess hormones, leading to symptoms like PMS, heavy bleeding, or irregular cycles.
Post-birth control recovery — After stopping hormonal contraception, it’s common for the body to take time to re-establish natural hormone communication — especially if nutrient stores were depleted.
The 8 Types of Abnormal Menstruation
Below is a table summarizing each type, followed by deeper insights into each.
| Type | What It Feels Like | Possible Causes |
|---|---|---|
| Amenorrhea | Missing your period for 3+ months, often with fatigue, hair thinning, or low libido. | Low energy availability, HPA axis suppression, post-pill, PCOS, thyroid dysfunction. |
| Oligomenorrhea | Infrequent or unpredictable cycles, with acne, mood swings, or trouble ovulating. | PCOS, under-eating, stress, thyroid issues. |
| Polymenorrhea | Bleeding more than once a month, often with short luteal phases and fatigue. | Anovulation, estrogen dominance, thyroid issues, fibroids, stress. |
| Menorrhagia | Very heavy periods or prolonged bleeding with clotting, cramps, and fatigue. | Hormone imbalance, fibroids, clotting disorders, thyroid dysfunction. |
| Hypomenorrhea | Light, short periods or spotting with low libido, short cycles, or fatigue. | Low estrogen, stress, under-eating, thyroid or hormonal suppression. |
| Dysmenorrhea | Severe cramping that may include nausea, headaches, and mood shifts. | High prostaglandins, inflammation, magnesium deficiency, endometriosis. |
| Metrorrhagia | Unexpected bleeding or spotting between periods, often with fatigue or anxiety. | Hormonal fluctuation, fibroids, IUDs, stress, thyroid imbalance. |
| PMS/PMDD | Emotional and physical symptoms before your period — from irritability to cravings. | Hormone sensitivity, serotonin imbalance, stress, nutritional deficiencies. |
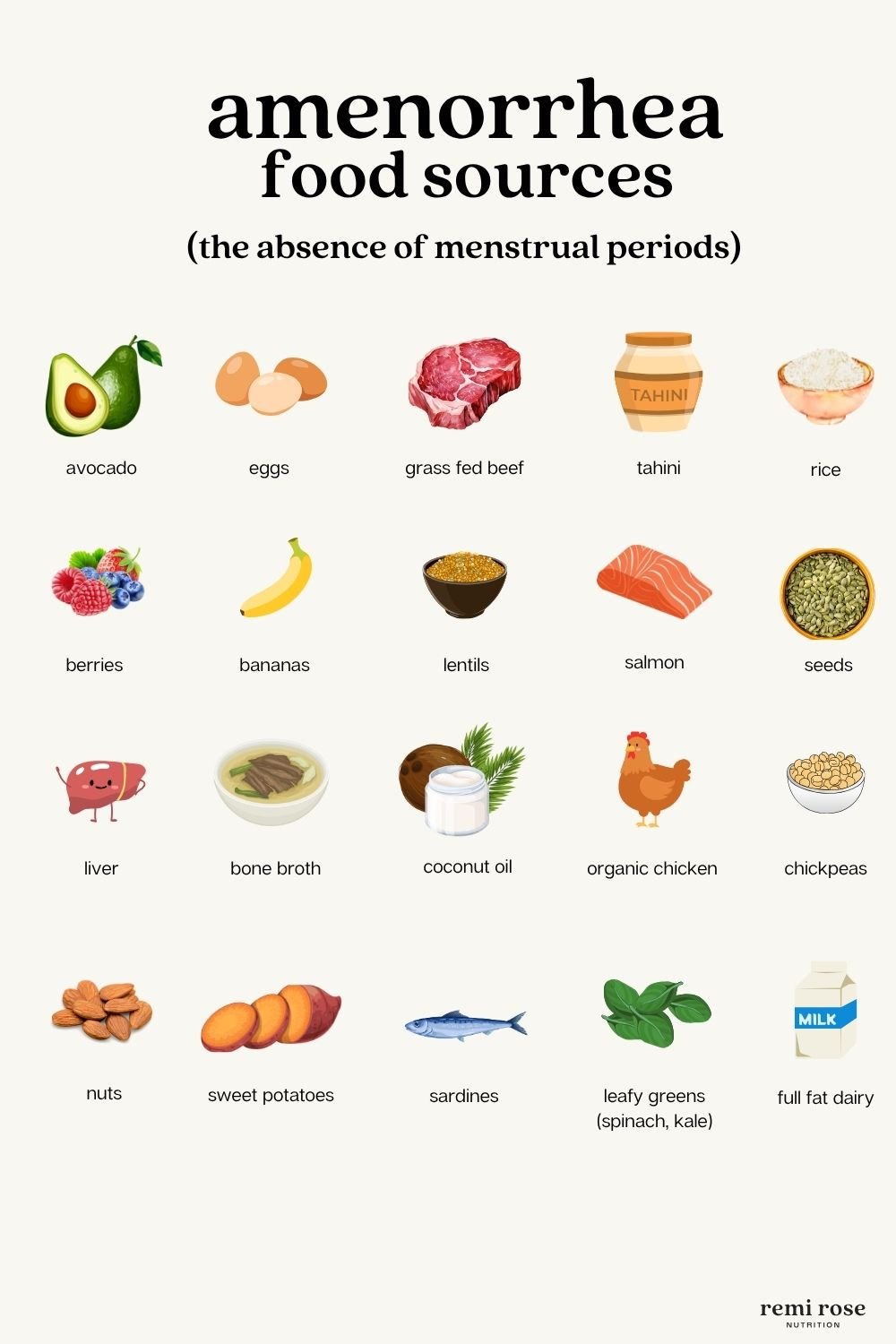
1. Amenorrhea (Absent or Missing Periods)
What it is: A missing or nonexistent period — typically for three months or more — that may come with fatigue, low body temperature, thinning hair, brittle nails, and a noticeable dip in libido or mood.
Possible Root Causes
Hypothalamic amenorrhea (often from under-eating or over-exercising)
Stress and elevated cortisol
Post-pill amenorrhea
PCOS or thyroid dysfunction
Holistic & Nutritional Support:
Eat enough: Energy deficiency is one of the most common root causes. Skipping meals or under-fueling (even unintentionally) can signal the brain to shut down reproductive function.
Include healthy fats with every meal: Think avocado, olive oil, nuts, seeds, and grass-fed butter.
Don’t skip carbs: Your body needs carbohydrates to ovulate and maintain a healthy cycle. Root vegetables, whole grains, and fruit are great options.
Minimize caffeine and alcohol, which can further stress your HPA axis and interfere with hormone production.
2. Oligomenorrhea (Infrequent or Irregular Periods)
What it is: A cycle that’s long, unpredictable, or tough to track — often accompanied by mood swings, acne, oily skin, increased body hair, and signs of delayed or inconsistent ovulation.
Possible causes:
PCOS
Under-eating or over-exercising
Stress and cortisol dysregulation
Thyroid issues
Holistic & Nutritional Support:
Balance blood sugar with every meal: Include protein, healthy fats, and fiber to support hormone production and insulin sensitivity.
Eat enough calories: Chronic under-eating suppresses the hypothalamic-pituitary-ovarian (HPO) axis.
Avoid ultra-processed foods and excess sugar, which cause hormonal rollercoasters.
Limit inflammatory oils (like canola and soybean) and replace with anti-inflammatory options like olive oil, avocado oil, and fatty fish.
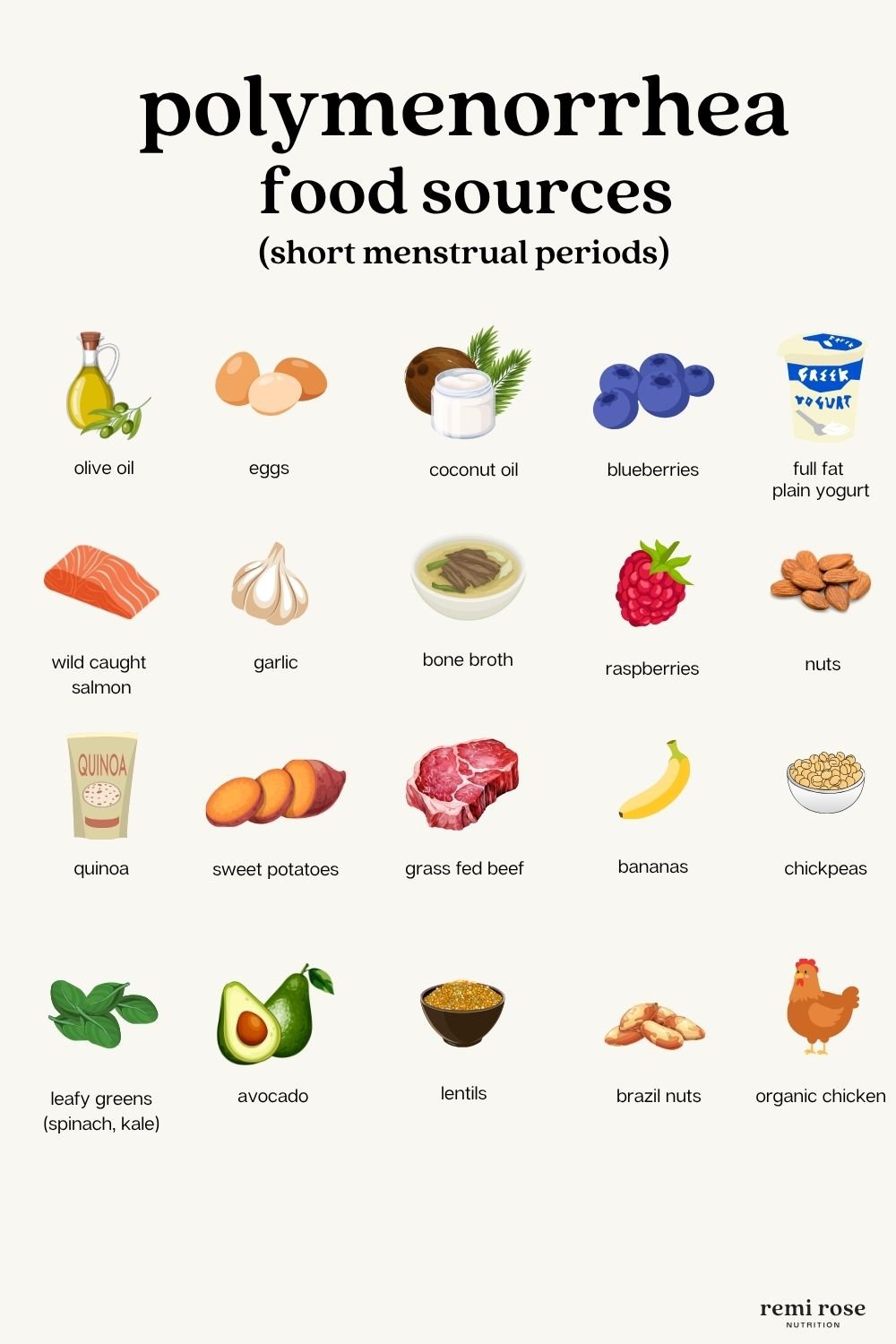
3. Polymenorrhea (Frequent or Closely Spaced Periods)
What it is: Short cycles occurring more than once every 21 days — often with fatigue from frequent bleeding, potential anemia, a shortened luteal phase, and stress or anxiety-related hormone flare-ups.
Possible causes:
Low progesterone or short luteal phase
Estrogen dominance
Perimenopause
Adrenal fatigue or chronic stress
Holistic & Nutritional Support:
Support progesterone naturally by including healthy fats, vitamin B6 (e.g., bananas, sunflower seeds), zinc (pumpkin seeds, beef), and vitamin C (citrus, peppers).
Replenish iron regularly through heme sources (meat, liver) and non-heme sources (lentils, spinach), ideally paired with vitamin C to enhance absorption.
Support liver detox with cruciferous veggies, garlic, fiber, and hydration.
Reduce caffeine, alcohol, and processed foods, all of which worsen hormone imbalances.
Consider adaptogens like maca or ashwagandha, especially if stress or adrenal fatigue is involved (consult a practitioner first).
4. Menorrhagia (Heavy or Prolonged Bleeding)
What it is: Periods lasting longer than 7 days or involving excessive blood loss — soaking through pads/tampons quickly or passing large clots — often accompanied by fatigue, dizziness, cramping, and anxiety around your period.
Possible causes:
Estrogen-progesterone imbalance
Uterine growths
Coagulation issues or medications
Infections or IUDs
Thyroid dysfunction
Holistic & Nutritional Support:
Eat iron-rich foods daily: Include heme iron (red meat, liver) and non-heme sources (lentils, tofu, spinach).
Pair iron-rich foods with vitamin C (like bell peppers, strawberries, lemon juice) for better absorption.
Support liver detox by increasing cruciferous vegetables (broccoli, Brussels sprouts), garlic, and fiber.
Reduce inflammation by avoiding processed sugar, alcohol, and inflammatory oils.
Add magnesium-rich foods (leafy greens, pumpkin seeds, dark chocolate) to reduce cramping and promote hormone balance.
5. Hypomenorrhea (Light or Short Periods)
What it is: Unusually light bleeding lasting just 1–2 days, often with minimal flow, shorter cycles, irregular ovulation, low libido, or fatigue.
Possible causes:
Low estrogen or underactive ovaries
Chronic under-eating or overexercising
Hormonal suppression (from stress, the pill, or nutrient deficiencies)
Psychological or physical stress
Holistic & Nutritional Support:
Prioritize calorie sufficiency: Restrictive eating or dieting can suppress ovulation and estrogen production.
Include healthy fats with every meal, such as avocados, nuts, seeds, olive oil, and ghee — your hormones are built from fat.
Don’t restrict carbs: Carbohydrates support ovulation and hormone production — opt for sweet potatoes, oats, quinoa, and fruit.
Replenish key nutrients like magnesium (leafy greens, dark chocolate), B vitamins (eggs, legumes), and zinc (pumpkin seeds, beef).
Limit caffeine and alcohol, which can further stress the hormonal system and suppress the HPA axis.
6. Dysmenorrhea (Painful Periods)
What it is: Intense menstrual cramps — often sharp or aching in the lower abdomen and back — that may include nausea, headaches, digestive upset, fatigue, mood shifts, and pain that sometimes requires medication.
Possible causes:
Elevated prostaglandins (inflammatory compounds)
Endometriosis or adenomyosis
Estrogen dominance or hormone imbalances
Magnesium or omega-3 deficiencies
Holistic & Nutritional Support:
Focus on anti-inflammatory foods: Load your plate with omega-3s (wild salmon, chia seeds), leafy greens, turmeric, and ginger.
Avoid pro-inflammatory foods, including processed sugar, seed oils (canola, soybean), and dairy (if not well tolerated).
Support magnesium intake to ease muscle tension and cramping — try pumpkin seeds, almonds, and leafy greens.
Support estrogen detoxification with cruciferous vegetables, plenty of fiber, and lots of hydration.
Keep blood sugar stable by eating balanced meals with protein, fiber, and healthy fats.
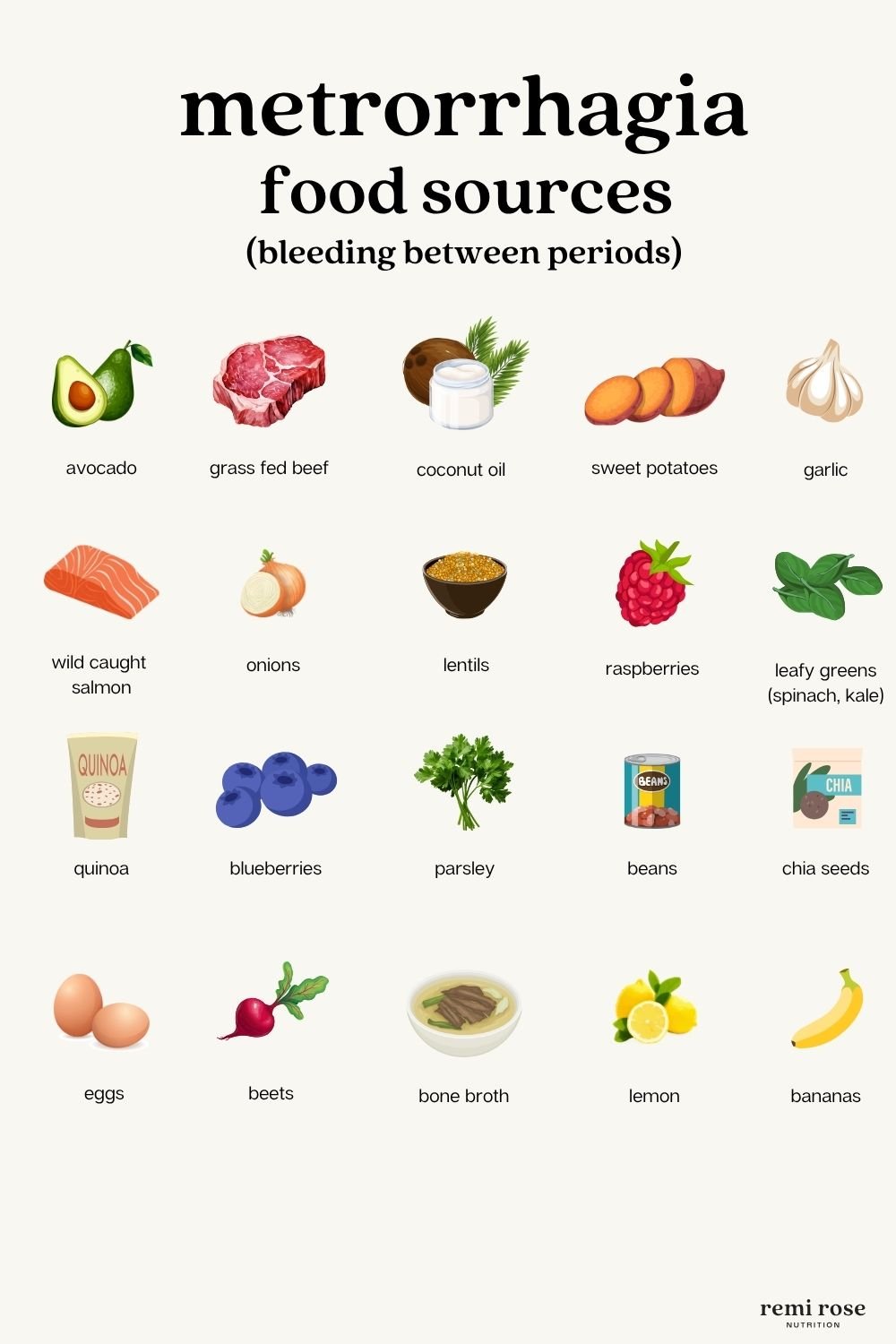
7. Metrorrhagia (Bleeding Between Periods)
What it is: Unexpected spotting or bleeding between regular cycles — often unpredictable, may cause fatigue or anemia, and can bring stress or mood changes.
Possible causes:
Hormone imbalances (e.g., low progesterone or estrogen dominance)
Coming off hormonal birth control
Uterine fibroids or endometrial issues
Perimenopause or stress
Clotting disorders
Holistic & Nutritional Support:
Support estrogen metabolism with liver-friendly foods like cruciferous veggies, garlic, and high-fiber meals.
Boost vitamin K for blood clotting support — include leafy greens, parsley, and full-fat yogurt (if tolerated).
Replenish iron and B vitamins lost through excess bleeding — focus on grass-fed meat, lentils, eggs, and leafy greens.
Balance hormones naturally using nutrients like vitamin E (avocado, sunflower seeds), zinc (pumpkin seeds), and B6 (chickpeas, tuna).
Avoid alcohol, caffeine, and processed sugar, which can stress the liver and worsen hormonal imbalances.
8. PMS/PMDD (Severe Premenstrual Symptoms)
What it is: Physical and emotional symptoms — such as mood swings, breast tenderness, fatigue, and irritability — that begin 1–2 weeks before your period. PMDD is a more intense form that can significantly disrupt your daily life.
Possible causes:
Sensitivity to normal hormone fluctuations
Serotonin imbalance
Genetic predisposition
Stress, smoking, or mood disorders
Blood sugar instability
Nutrient deficiencies (magnesium, B6, calcium)
Holistic & Nutritional Support:
Balance blood sugar: Eat every 3–4 hours and make sure meals include protein, fat, and fiber to stabilize energy and mood.
Support serotonin with tryptophan-rich foods (eggs, turkey, bananas) + vitamin B6 to assist neurotransmitter production.
Increase magnesium, calcium, B6, and omega-3s through whole foods or supplements to ease both emotional and physical symptoms.
Avoid processed sugar, alcohol, and caffeine — these can spike cortisol, dysregulate blood sugar, and worsen PMS symptoms.
Support estrogen detoxification using cruciferous veggies, fiber, lemon water, and gentle liver-supporting herbs or foods.
Foods That Support Hormone Balance and a Regular Cycle
Supporting your cycle isn’t about quick fixes — it’s about building a stable, well-fed internal environment. Here are some fundamentals:
Key Nutrients for Cycle Health
Magnesium: Eases cramps and supports progesterone
Zinc: Crucial for ovulation and cycle regularity
Iron: Replenishes after blood loss
B Vitamins: Fuel detox and hormone metabolism
Omega-3s: Reduce inflammation and support hormone production
I also recommend an herbal supplement like Cycle Balance, which works to support menstrual discomforts and their underlying patterns.





Cycle-Friendly Lifestyle Habits to Support Hormonal Balance.
Nutrition lays the foundation, but daily habits play a key role in maintaining a healthy, regular cycle. Here are the most impactful lifestyle practices to support hormonal balance:
Eat enough and eat consistently: Undereating or skipping meals can suppress ovulation and throw off your cycle.
Prioritize rest and recovery: Chronic stress and poor sleep disrupt hormone communication — aim for 7–9 hours nightly.
Balance blood sugar daily: Include protein, fat, and fiber at every meal to stabilize mood and support hormone production.
Limit alcohol, caffeine, and processed foods: These can spike cortisol, burden your liver, and worsen PMS symptoms.
Support liver and gut health: Cruciferous veggies, hydration, and regular bowel movements help clear excess estrogen.
Track your cycle: Awareness helps you spot imbalances early and align habits with your hormonal rhythm.
Looking For Individual Support?
Irregular periods are more common than you think — but that doesn’t mean they’re normal. Your menstrual cycle is your body’s monthly report card. It’s not something to suppress, but to listen to.
If you’re ready to dig deeper and support your cycle naturally, consider my three-month Hormone Balancing Program. It provides one-on-one support to guide your healing process, with nutrition education, holistic counseling, personalized meal planning, and more.
You can also check out my guide The Effects of Birth Control — & How to Transition Off It, which includes a 6-week hormone-balancing meal plan, grocery lists, daily tips, and recipes to help you restore your cycle — whether you’re post-pill or simply trying to feel better.




